2023-03-30T12:05:00
(BPT) – The story you are about to read may not be representative of all people living with schizophrenia. The opinions expressed here are those of Robert, a person living with schizophrenia, and are not a substitute for medical advice or judgment. Always talk to your doctor/healthcare provider (HCP) about available and appropriate treatment options. Individual results may vary.
My life for three decades had been a struggle. I was living on the streets, found it hard to hold a job, and had symptoms—like hearing voices—that I didn’t understand. What I didn’t know until I was diagnosed by a healthcare provider is that I was living with schizophrenia, a serious mental health condition that affects about one percent of the U.S. population.1
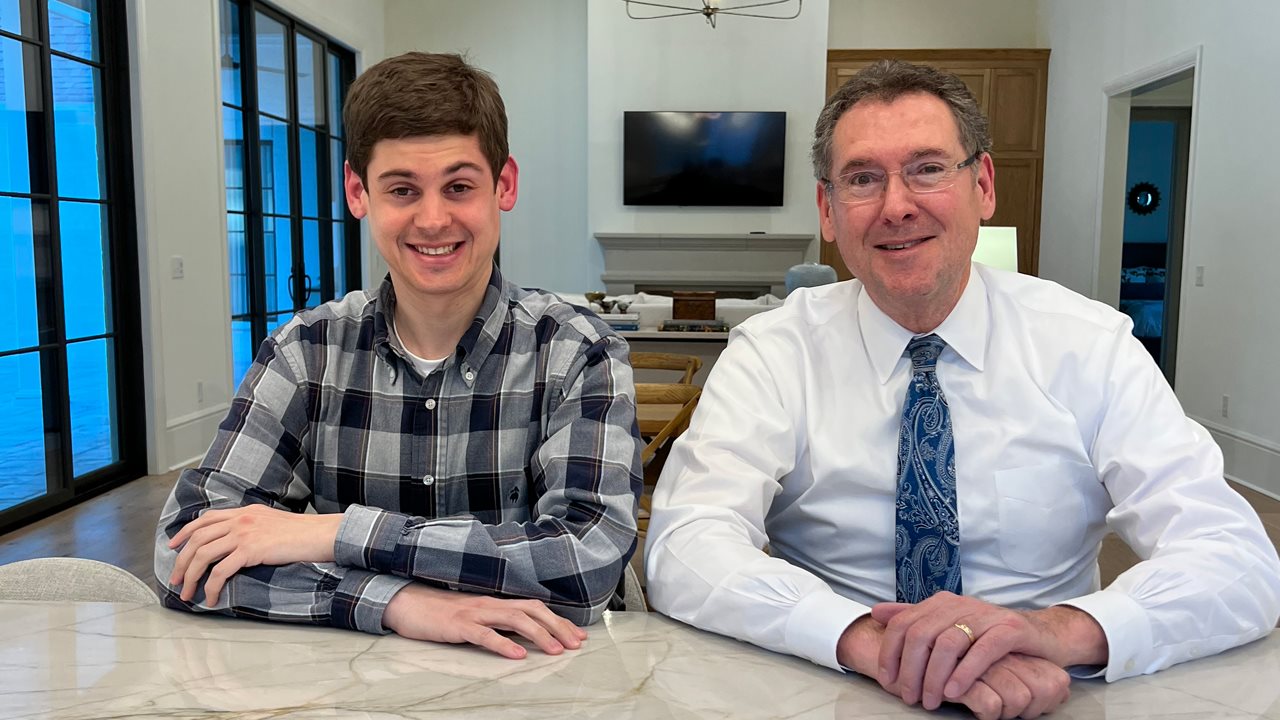
When I first met Scott, I was carrying all my possessions around on my bike. Scott often reminds me that despite my tough situation, he was amazed at the big smile on my face. That chance meeting turned into a lifelong friendship that would set me on a new path.
At the time we met, Scott was on an extended trip to California visiting his son in college. Later that week, Scott offered to buy me a croissant and a cup of coffee, and I accepted.
Life for me at that time was difficult. I had a hard time staying in one place for too long and struggled making decisions, but I was convinced that this was just a result of being “unhoused.” It never occurred to me that I could be struggling from a serious mental illness.
As time went on, it was sometimes challenging for me to tell the difference between real and imaginary dangers, and there were times when I would hear voices that weren’t there. I thought that my mental health may be a problem, but I had no connections or resources to ask for help. I thought I could use a friend, and Scott became that for me. The more time he spent getting to know me, the more I trusted him. Over many coffees and croissants, we shared stories about our lives and learned that we had some important things in common.
Over the next several months, Scott travelled back and forth between Rhode Island and California and we continued to build our friendship. He even spent a night sleeping in a parking garage with me—he wanted me to know that I had an ally in him. I did not know this at the time, but Scott had done some of his own research about support options that could be available to me. So when he eventually offered to help me find an HCP for a potential evaluation, I was ready.
My acceptance of Scott’s offer of help was influenced by his compassion and support for my well-being. Scott went with me to a mental health center where, after a full evaluation, an HCP formally diagnosed me with schizophrenia. Some of the symptoms of schizophrenia may include, but are not limited to, hallucinations, delusions, difficulty functioning normally, trouble focusing and behaviors associated with psychosis.2 Most people living with schizophrenia will require an integrated approach to treatment that includes medication, therapy, and psychosocial support to manage their condition.3
After talking to my doctor about my treatment options, we decided that ARISTADA® (aripiprozole lauroxil) may be a good choice for my schizophrenia treatment journey. ARISTADA is a prescription medicine used to treat schizophrenia in adults and is given via injection by a healthcare professional. After establishing tolerability to aripiprozole and completing treatment initiation, I began taking the 2-month (1064 mg) dose of ARISTADA.4,5
Here is some important safety information about ARISTADA: It is not known if ARISTADA is safe and effective in patients under 18. It’s also important to know that elderly people with dementia-related psychosis are at increased risk of death when treated with antipsychotic medicines including ARISTADA. ARISTADA is not for the treatment of people who have lost touch with reality (psychosis) due to confusion and memory loss (dementia). The most common side effects of ARISTADA include restlessness or feeling like you need to move (akathisia).5 These are not all of the side effects associated with ARISTADA. For additional Important Safety Information, please see below.
Since starting on ARISTADA, I have noticed an improvement in my schizophrenia symptoms. This has just been my experience and yours may be different. Talk to your healthcare team about what may be best for you.
After helping me seek treatment, Scott went back to Rhode Island, but we talked every day. On one occasion, I expressed wanting to move to New England and Scott was supportive of the idea—it was one of the biggest decisions on my journey.
In our search for my permanent home, Scott found a cabin about 45 minutes away from his house. I packed a bag and moved across the country. It was the first time in many years that I had a place of my own. When I woke up the next morning in my bed, I knew I was finally home.
No matter what the future holds, I maintain a dialogue with my care team and stick with my treatment plan with the support of Scott and my healthcare providers.
This is intended as informational only and not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical and/or mental health condition.
Please read the Important Safety Information for ARISTADA INITIO® and ARISTADA below. Discuss all benefits and risks with a healthcare provider. See Prescribing Information for ARISTADA INITIO and ARISTADA, including Boxed Warning, and Medication Guides for ARISTADA INITIO and ARISTADA.
INDICATION and IMPORTANT SAFETY INFORMATION for ARISTADA INITIO® (aripiprazole lauroxil) and ARISTADA® (aripiprazole lauroxil) extended-release injectable suspension, for intramuscular use
INDICATION
ARISTADA INITIO is a prescription medicine given as a one-time injection and is used in combination with oral aripiprazole to start ARISTADA treatment, or re-start ARISTADA treatment after a missed dose, when ARISTADA is used for the treatment of schizophrenia in adults.
ARISTADA is a prescription medicine given by injection by a healthcare professional and used to treat schizophrenia in adults.
It is not known if ARISTADA INITIO and/or ARISTADA are safe and effective in children under 18 years of age.
IMPORTANT SAFETY INFORMATION
|
Elderly people with dementia-related psychosis are at increased risk of death when treated with antipsychotic medicines including ARISTADA INITIO and ARISTADA. ARISTADA INITIO and ARISTADA are not for the treatment of people who have lost touch with reality (psychosis) due to confusion and memory loss (dementia).
|
Contraindication: Do not receive ARISTADA INITIO or ARISTADA if you are allergic to aripiprazole or any of the ingredients in ARISTADA. Allergic reactions to aripiprazole have ranged from rash, hives and itching to anaphylaxis, which may include difficulty breathing, tightness in the chest, and swelling of the mouth, face, lips, or tongue.
ARISTADA INITIO and/or ARISTADA may cause serious side effects including:
- Cerebrovascular problems (including stroke) in elderly people with dementia-related psychosis that can lead to death.
- Neuroleptic malignant syndrome (NMS), a serious condition that can lead to death. Call your healthcare provider or go to the nearest hospital emergency room right away if you have some or all of the following signs and symptoms of NMS:
- high fever
- stiff muscles
- confusion
- sweating
- changes in pulse, heart rate, and blood pressure
- Uncontrolled body movements (tardive dyskinesia). ARISTADA INITIO and ARISTADA may cause movements that you cannot control in your face, tongue, or other body parts. Tardive dyskinesia may not go away, even if you stop receiving ARISTADA. Tardive dyskinesia may also start after you stop receiving ARISTADA.
- Problems with your metabolism such as:
- High blood sugar (hyperglycemia). Increases in blood sugar can happen in some people who receive ARISTADA INITIO and/or ARISTADA. Extremely high blood sugar can lead to coma or death. If you have diabetes or risk factors for diabetes (such as being overweight or a family history of diabetes), your healthcare provider should check your blood sugar before you receive ARISTADA INITIO and/or ARISTADA and during your treatment with ARISTADA.
- Call your healthcare provider if you have any of these symptoms of high blood sugar:
- feel very thirsty
- need to urinate more than usual
- feel very hungry
- feel weak or tired
- feel sick to your stomach
- feel confused, or your breath smells fruity
- Increased fat levels (cholesterol and triglycerides) in your blood
- Weight gain. You and your healthcare provider should check your weight regularly.
- Unusual and uncontrollable (compulsive) urges. Some people taking aripiprazole have had strong unusual urges such as gambling that cannot be controlled (compulsive gambling). Other compulsive urges include sexual urges, shopping, and eating or binge eating. If you or your family members notice that you are having unusual strong urges, talk to your healthcare provider.
- Decreased blood pressure (orthostatic hypotension). You may feel lightheaded or faint when you rise too quickly from a sitting or lying position.
- Falls. ARISTADA INITIO and ARISTADA may make you sleepy or dizzy when standing which may make you at risk for falls and related injuries
- Low white blood cell count
- Seizures (convulsions)
- Problems controlling your body temperature. Avoid becoming too hot or dehydrated. Do not exercise too much. In hot weather, stay inside in a cool place if possible. Stay out of the sun. Do not wear too much clothing or heavy clothing. Drink plenty of water.
- Difficulty swallowing
The most common side effects of ARISTADA INITIO and ARISTADA include restlessness or feeling like you need to move (akathisia). These are not all the possible side effects of ARISTADA INITIO and ARISTADA. You should tell your healthcare provider about any side-effects you have.
Do not drive, operate hazardous machinery, or do other dangerous activities until you know how ARISTADA INITIO and ARISTADA affect you. ARISTADA INITIO and ARISTADA may affect your judgment, thinking or motor skills.
Before receiving ARISTADA INITIO and ARISTADA tell your healthcare provider about all of your medical conditions, including if you:
- have not taken Abilify®, Abilify Maintena®, or any aripiprazole product before
- have or had heart problems or a stroke
- have diabetes or high blood sugar or a family history of diabetes or high blood sugar. Your healthcare provider should check your blood sugar before you receive ARISTADA INITIO and/or ARISTADA and during your treatment with ARISTADA
- have or had low or high blood pressure
- have or had seizures (convulsions)
- have or had a low white blood cell count
- have problems that may affect you receiving an injection in your buttocks or your arm
- are pregnant or plan to become pregnant. It is not known if ARISTADA INITIO and/or ARISTADA will harm your unborn baby. If you become pregnant while taking ARISTADA INITIO and/or ARISTADA, talk to your healthcare provider about registering with the National Pregnancy Registry for Atypical Antipsychotics. You can register by calling
1-866-961-2388, or visit http://womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry/
- are breastfeeding or plan to breastfeed. ARISTADA INITIO and/or ARISTADA can pass into your breast milk. It is not known if it may harm your baby. Talk to your healthcare provider about the best way to feed your baby if you receive ARISTADA INITIO and/or ARISTADA.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. ARISTADA INITIO and ARISTADA and other medicines may affect each other causing possible serious side effects. Do not start or stop any medicines after you receive ARISTADA INITIO and ARISTADA without talking to your healthcare provider first.
|
If you have any questions about your health or medicines, talk to your healthcare provider. You are encouraged to report all side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch, or call 1-800-FDA-1088.
|
References:
1 Cloutier M, Aigbogun MS, Guerin A, et al. The Economic Burden of Schizophrenia in the United States in 2013. J Clin Psychiatry. 2016;77(6):764-771. doi:10.4088/JCP.15m10278
2 American Psychiatric Association. Schizophrenia Spectrum and Other Psychiatric Disorders. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
3 Schizophrenia Fact Sheet. National Alliance on Mental Illness (NAMI). Accessed January 26, 2023. https://www.nami.org/NAMI/media/NAMI-Media/Images/FactSheets/Schizophrenia-FS.pdf
4 ARISTADA [Medication Guide]. Waltham, MA: Alkermes, Inc.; 2021.
5 ARISTADA [Prescribing Information]. Waltham, MA: Alkermes, Inc.; 2021.
ALKERMES® is a registered trademark of Alkermes, Inc. ARISTADA® and logo, and ARISTADA INITIO®, are registered trademarks of Alkermes Pharma Ireland Limited, used by Alkermes, Inc., under license. Abilify® is a trademark of Otsuka Pharmaceutical Company and Abilify Maintena® is a trademark of Otsuka Pharmaceutical Co., Ltd. ©2023 Alkermes, Inc. All rights reserved. ARI-004930.