2024-09-27T08:01:00
(BPT) – Sponsored by Novartis Pharmaceuticals Corporation
Did you know that in the US, nearly half of all adults have some type of cardiovascular disease (CVD), also referred to as known heart disease?[1] A common type of heart disease, called atherosclerotic cardiovascular disease (ASCVD), is caused by consistent high levels of “bad cholesterol” (aka, low density lipoprotein cholesterol or LDL-C).[2],[3] Prolonged exposure to high levels of bad cholesterol can result in the formation of plaque, which can lead to blockages that can increase the risk of heart attack or stroke.[2],[3] The problem? Many people may not know this vital information or how to manage high levels of bad cholesterol.
Bad cholesterol can be measured through a standard lipid panel, which can be done at a healthcare provider’s office.[4] But the reality is that one in five heart attacks that occur in the US are silent, meaning the damage was done without the person knowing.[5] One reason this may happen is because high levels of bad cholesterol can be a symptomless condition — that is why it’s critical for everyone to be aware of their bad cholesterol levels, and if they are high, take proactive steps to reduce their bad cholesterol.[3]
Bringing the Connection to Life
Richard is an active person who likes to fish, work on his home landscaping projects, and play with his son. Coming from a family with a long history of heart disease, Richard always knew he had to be proactive and take his health seriously. But despite his best efforts with diet and an active lifestyle, healthcare providers found a 95% blockage in his left anterior descending artery, also known as the “widowmaker.”[6]
“This significant of a blockage, created by plaque build-up as a result of consistently high levels of bad cholesterol, can cause fatal heart events, hence the name ‘widowmaker,’” says Nicole Ciffone, Nurse Practitioner, Lipid Specialist and Founder of Arizona Lipid Center. “Richard’s proactivity around managing his health might have just saved his life, but many patients don’t know that consistently high levels of bad cholesterol can put them at serious risk for a cardiac event.”
To reduce the blockage and increase blood flow, Richard’s care team placed a stent into his heart, followed by three more over the next six years. Stents are placed in arteries to keep the artery from narrowing or closing.[7] During this time, Richard and his cardiologist kept a close eye on his bad cholesterol levels, which remained high.
After recovering from cardiac surgery, Richard was prescribed statins, a common cholesterol medication, and continued to prioritize a healthy diet and exercise routine.[8]
A Turning Point
“I was doing everything right, but my bad cholesterol remained higher than it should be, even after I started statin therapy,” recalls Richard.
“When you’re already doing everything you think you can do to manage or lower bad cholesterol, not seeing those numbers go down can be frustrating,” said Ciffone. “Sometimes a cholesterol-lowering treatment like statins, even when paired with a healthy lifestyle, isn’t enough.”
Determined not to let his challenges with managing his bad cholesterol impact his most important role in life, being a parent to his young son, Richard worked proactively with his healthcare team to find a treatment to lower his bad cholesterol, which included the addition of non-statin therapy. Richard was prescribed an injectable treatment called Leqvio® (inclisiran), which works with the liver’s natural process to support the lowering of bad cholesterol, along with diet and a statin.[9]
After an initial dose, followed by one at three months, it’s administered by a health care provider twice-yearly.[9] In clinical studies it has been shown to help lower bad cholesterol by about 50% and keep it low through each six-month dosing interval at 17 months.[9]
“I’ve been taking Leqvio for one year now and have been able to reduce my bad cholesterol to levels both me and my healthcare provider are happy with,” Richard said. “It’s been nice to see my numbers go down after years of struggle. And for me and my lifestyle, it’s nice to not have to remember to take another medication or self-inject.”
Finding a Treatment that Works for You
“Leqvio is another great tool in our toolbox to help patients lower their bad cholesterol levels, along with diet and statins,” said Ciffone. “The twice-yearly dosing, after two initial doses, and HCP administration may work for some patients’ lifestyle. But, it’s important that patients speak with their own healthcare providers about what treatment option may be right for them.”
The most common side effects of Leqvio include injection site reaction (including pain, redness, and rash), joint pain, and chest cold.[9] Please see additional safety information below. It is not known if Leqvio can decrease problems related to high cholesterol, such as heart attacks or stroke.[9]
Bad cholesterol can be a symptomless condition, which can make it easy to forget or ignore as patients may be prioritizing other health conditions.[3] However, managing bad cholesterol is extremely important, especially for patients who are considered “high-risk” for heart disease.
“It’s understandable, given the overwhelming amount of change a patient may need to adopt, that some patients and providers may not prioritize getting to LDL-C guideline recommended thresholds,” said Ciffone. “I encourage both patients and the community of healthcare providers to remain vigilant on bad cholesterol management throughout a patient’s healthcare journey.”
Opportunities for Others
“I hope sharing my story and acknowledging some of the challenges I’ve faced managing my bad cholesterol can help others,” shares Richard. It’s critical to know the status of your bad cholesterol and lower it to the recommended goal and keep it low.[10] By talking to his healthcare providers, Richard was able to find a treatment option that worked for him.
To prepare for these conversations you should understand your target LDL-C number. For example, for patients who have experienced a heart attack or stroke the American Heart Association recommends LDL-C levels of 70 mg/dL or lower.[11]
“If people knew about the importance of managing bad cholesterol, they would take a more proactive approach and have those important conversations with their healthcare providers early,” says Richard.
If you or a loved one has continued to struggle with high LDL-C, despite statin therapy and lifestyle changes, it’s important to ask your healthcare provider about other treatment options.
To learn more about Leqvio, visit Leqvio.com.
What is LEQVIO?
LEQVIO (inclisiran) is an injectable prescription medicine used along with diet and other cholesterol-lowering medicines in adults with high blood cholesterol levels called primary hyperlipidemia (including a type of high cholesterol called heterozygous familial hypercholesterolemia [HeFH]) to reduce low-density lipoprotein (LDL-C) or “bad” cholesterol.
IMPORTANT SAFETY INFORMATION
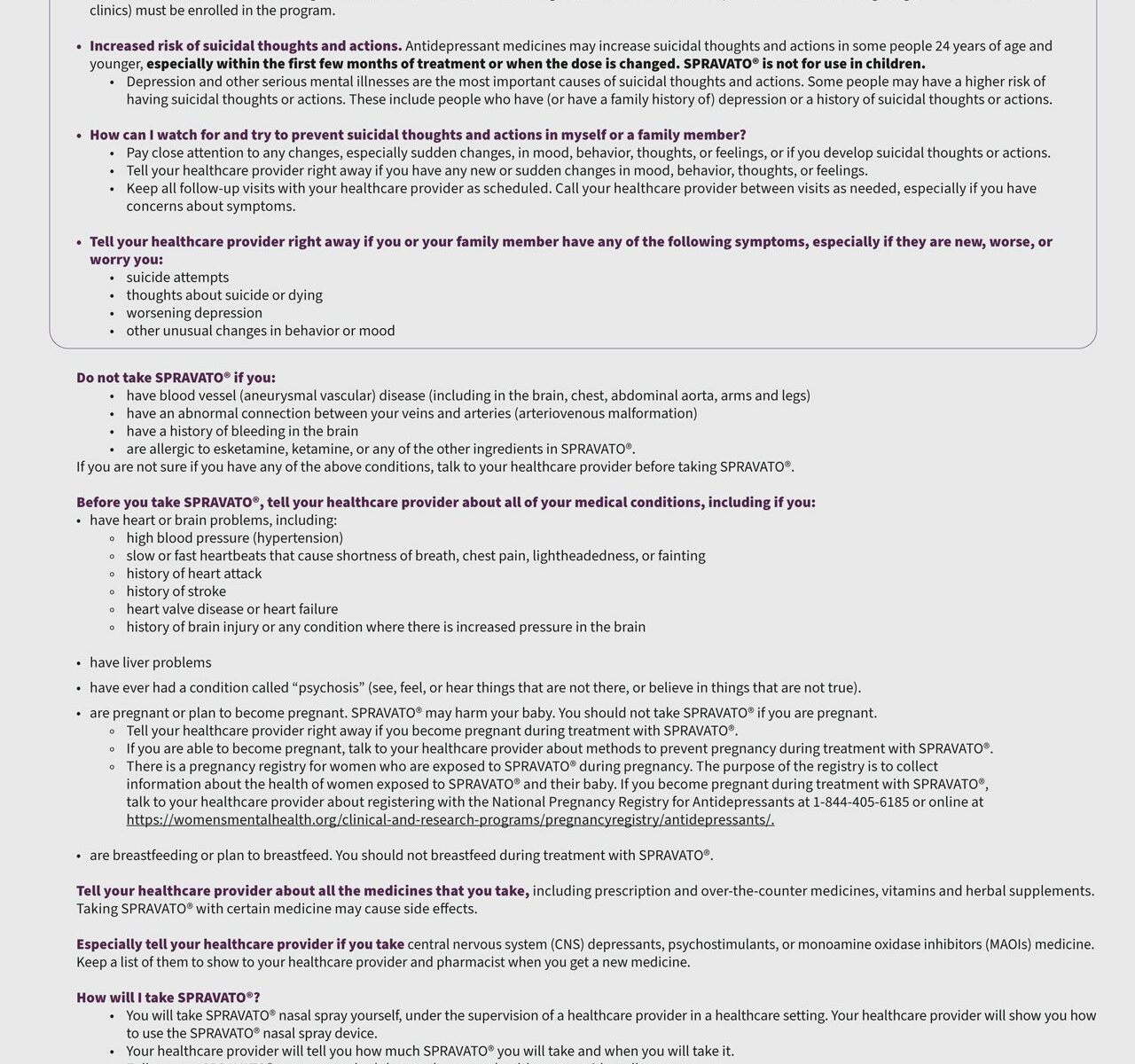
Do not use if you have had an allergic reaction to LEQVIO or any of its ingredients.
The most common side effects of LEQVIO were: injection site reaction (including pain, redness, and rash), joint pain, and chest cold.
These are not all the possible side effects of LEQVIO. Ask your healthcare provider for medical advice about side effects. You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch, or call 1-800-FDA-1088.
Please click here for accompanying LEQVIO full Prescribing Information.
References
[1] Martin SS, Aday AW, Almarzooq ZI, et al. 2024 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association. Circulation. 2024; 149(8):e347-e913. doi: 10.1161/CIR.0000000000001209
[9] Leqvio [prescribing Information]. East Hanover, NJ: Novartis Pharmaceuticals Corp; 2024.
[10] Mhaimeed O, Burney ZA, Schott SL, et al. The importance of LDL-C lowering in atherosclerotic cardiovascular disease prevention: Lower for longer is better. Am J Prev Cardiol. 2024; 18:100649. doi:10.1016/j.ajpc.2024.100649
[11] Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019 Jun 18;139(25):e1082-e1143. doi: 10.1161/CIR.0000000000000625.
9/24 FA-11248272