2024-08-21T08:01:00
(BPT) – Many people think of eczema as a mild, itchy skin disease, and don’t realize how intense signs and symptoms can become. However, those living with moderate-to-severe forms of the condition know that it’s much more than that. They can experience recurring signs and symptoms such as intense itching and dry, irritating rashes that can crack or ooze. The discomfort is present throughout their daily activities — whether working, practicing, or spending time with loved ones.
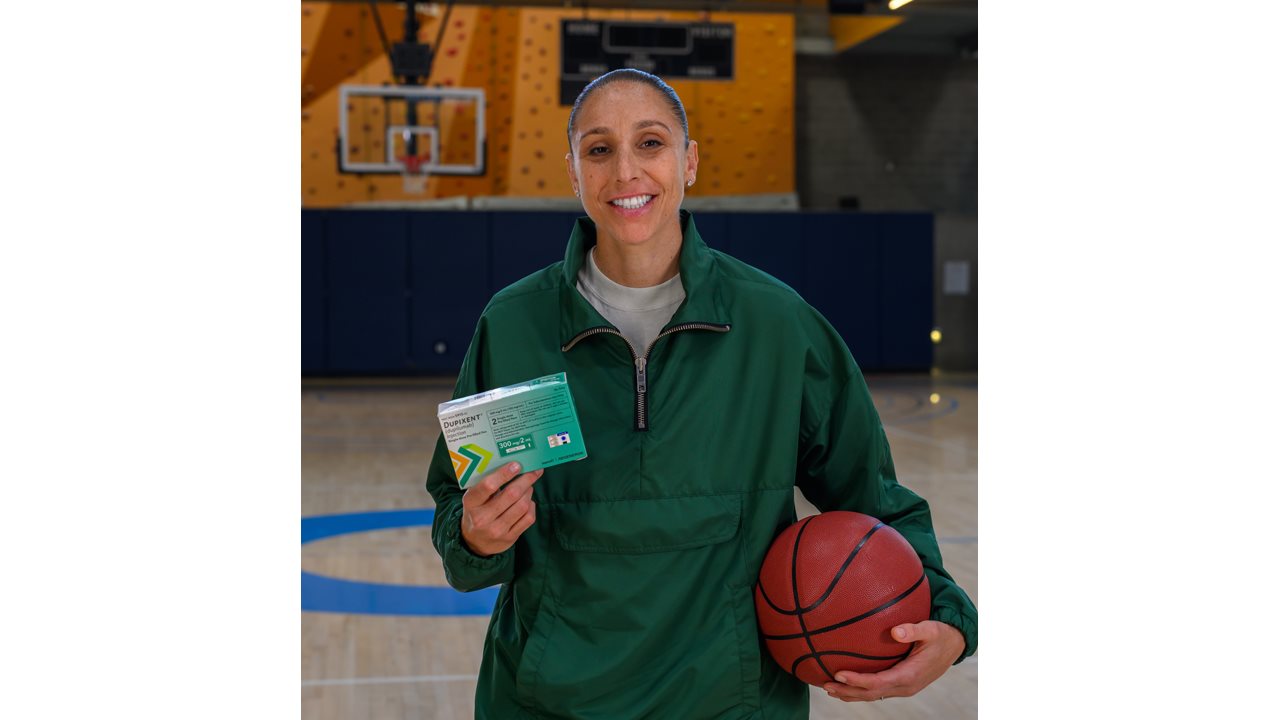
Diana Taurasi, all-star basketball player, has been living with moderate-to-severe eczema since her college days, and is aware of the challenges it can bring both on and off the court. In partnership with Sanofi and Regeneron for the Eczactly Like Me program, Diana is ready to share her story to help others living with the disease recognize that they’re not alone in their struggles.
Diana’s Moderate-to-Severe Eczema Journey
Diana first noticed signs and symptoms of moderate-to-severe eczema that manifested as rashes on her arms and hands while playing basketball in college.
“Playing a sport where a lot of your skin is exposed, I’m in this constant cycle of sweating, showering, and drying off, all things that can irritate my skin. There were times when my skin was so itchy, I’d get in the shower and make the water as hot as I could stand it just to get some temporary relief — but in the long run, it would just make my itchy skin feel worse.”
Throughout the years, she was constantly dealing with her itchy skin, and her eczema was often on her mind. “I was one of the first players in the league to wear long sleeves, and it was to hide my skin, which people probably didn’t know.”
Outside of basketball, certain activities could be tough on Diana’s skin, even while spending time with friends and family. While on vacation for example, she’d sometimes avoid going to the pool or being out in the heat because of how it would irritate her skin.
Finding A Treatment That Works for Her
Diana worked with her dermatologist to try different prescription topical treatments but her eczema still wasn’t well controlled.
“I started to feel hopeless about my skin and like I might never find something that would work for me.”
Eventually, her doctor recommended she try Dupixent (dupilumab), a biologic treatment option for people ages 6 months and older with uncontrolled moderate-to-severe eczema.
Dupixent works by helping to block a key source of inflammation inside the body, to help reduce itch and rashes. It is the only biologic medicine approved to treat uncontrolled moderate-to-severe eczema from infancy to adulthood.
Since starting Dupixent, Diana reported experiencing clearer skin and less itch.
“I spent years not knowing there could be a treatment out there that could work for me. Now, I feel like I’ve got the ball in this never-ending match against my moderate-to-severe eczema. I’m enjoying doing things like swimming with my wife and kids, but without being as worried about my eczema. While every person is different, this was my experience.”
Dupixent can help adult patients with moderate-to-severe eczema achieve clearer skin and less itch. In two clinical trials at 16 weeks, adults on Dupixent had clear or almost clear skin (37% vs 9% not on Dupixent) and significant itch reduction (38% vs 11% not on Dupixent). Individual results may vary.
The most common side effects include injection site reactions, eye and eyelid inflammation, including redness, swelling, and itching, sometimes with blurred vision, dry eye, cold sores in your mouth or on your lips, and high count of a certain white blood cell (eosinophilia).
Advice For Others “Eczactly” Like Diana Living with Moderate-to-Severe Eczema
Diana wants other people out there who feel “Eczactly” like her and going through similar challenges with moderate-to-severe eczema to not lose hope.
“If you or a loved one has uncontrolled moderate-to-severe eczema, you’re not alone — there’s a lot of people out there dealing with similar struggles because of this disease. Don’t give up — it’s important to advocate for yourself or your loved one and to talk to a dermatologist about treatment options.”
Visit ShowUpAD.com to learn more about stories like Diana’s and learn more about Dupixent(dupilumab).
IMPORTANT SAFETY INFORMATION & INDICATION
Do not use if you are allergic to dupilumab or to any of the ingredients in DUPIXENT®.
Before using DUPIXENT, tell your healthcare provider about all your medical conditions, including if you:
- have eye problems.
- have a parasitic (helminth) infection.
- are scheduled to receive any vaccinations. You should not receive a “live vaccine” right before and during treatment with DUPIXENT.
- are pregnant or plan to become pregnant. It is not known whether DUPIXENT will harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known whether DUPIXENT passes into your breast milk.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Especially tell your healthcare provider if you are taking oral, topical or inhaled corticosteroid medicines or if you have atopic dermatitis and asthma and use an asthma medicine. Do not change or stop your corticosteroid medicine or other asthma medicine without talking to your healthcare provider. This may cause other symptoms that were controlled by the corticosteroid medicine or other asthma medicine to come back.
DUPIXENT can cause serious side effects, including:
- Allergic reactions. DUPIXENT can cause allergic reactions that can sometimes be severe. Stop using DUPIXENT and tell your healthcare provider or get emergency help right away if you get any of the following signs or symptoms: breathing problems or wheezing, swelling of the face, lips, mouth, tongue, or throat, fainting, dizziness, feeling lightheaded, fast pulse, fever, hives, joint pain, general ill feeling, itching, skin rash, swollen lymph nodes, nausea or vomiting, or cramps in your stomach-area.
- Eye problems. Tell your healthcare provider if you have any new or worsening eye problems, including eye pain or changes in vision, such as blurred vision. Your healthcare provider may send you to an ophthalmologist for an eye exam if needed.
- Joint aches and pain. Some people who use DUPIXENT have had trouble walking or moving due to their joint symptoms, and in some cases needed to be hospitalized. Tell your healthcare provider about any new or worsening joint symptoms. Your healthcare provider may stop DUPIXENT if you develop joint symptoms.
The most common side effects in patients with eczema include injection site reactions, eye and eyelid inflammation, including redness, swelling, and itching, sometimes with blurred vision, dry eye, cold sores in your mouth or on your lips, and high count of a certain white blood cell (eosinophilia).
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of DUPIXENT. Call your doctor for medical advice about side effects. You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch, or call 1-800-FDA-1088.
Use DUPIXENT exactly as prescribed by your healthcare provider. It’s an injection given under the skin (subcutaneous injection). Your healthcare provider will decide if you or your caregiver can inject DUPIXENT. Do not try to prepare and inject DUPIXENT until you or your caregiver have been trained by your healthcare provider. In children 12 years of age and older, it’s recommended DUPIXENT be administered by or under supervision of an adult. In children 6 months to less than 12 years of age, DUPIXENT should be given by a caregiver.
Please see accompanying full Prescribing Information including Patient Information.
INDICATION
DUPIXENT is a prescription medicine used to treat adults and children 6 months of age and older with moderate-to-severe eczema (atopic dermatitis or AD) that is not well controlled with prescription therapies used on the skin (topical), or who cannot use topical therapies. DUPIXENT can be used with or without topical corticosteroids. It is not known if DUPIXENT is safe and effective in children with atopic dermatitis under 6 months of age.
US.DUP.24.06.0421