2024-08-14T08:01:00
(BPT) – CDKL5 deficiency disorder, one of the most common genetic epilepsies, is estimated to occur in approximately 100 newborns in the U.S. per year.
CDKL5 deficiency disorder, or CDD, is a rare, X-linked developmental and epileptic encephalopathy characterized by refractory seizures and severe global developmental impairment. The frequency of seizures related to CDD can vary, with some patients experiencing up to 20 seizures a day.
Those diagnosed with CDD face many challenges living with a rare disease and can experience a wide range of chronically debilitating symptoms, including early-onset seizures, global developmental impairment, and intellectual disability, as well as disorders related to sleep, speech, physical development, and cortical vision.
Although there is currently no cure for CDD, research into better understanding the disease and the development of treatment options continues to advance. In fact, in 2022 the FDA approved the first treatment specifically for seizures associated with CDD in appropriate patients.
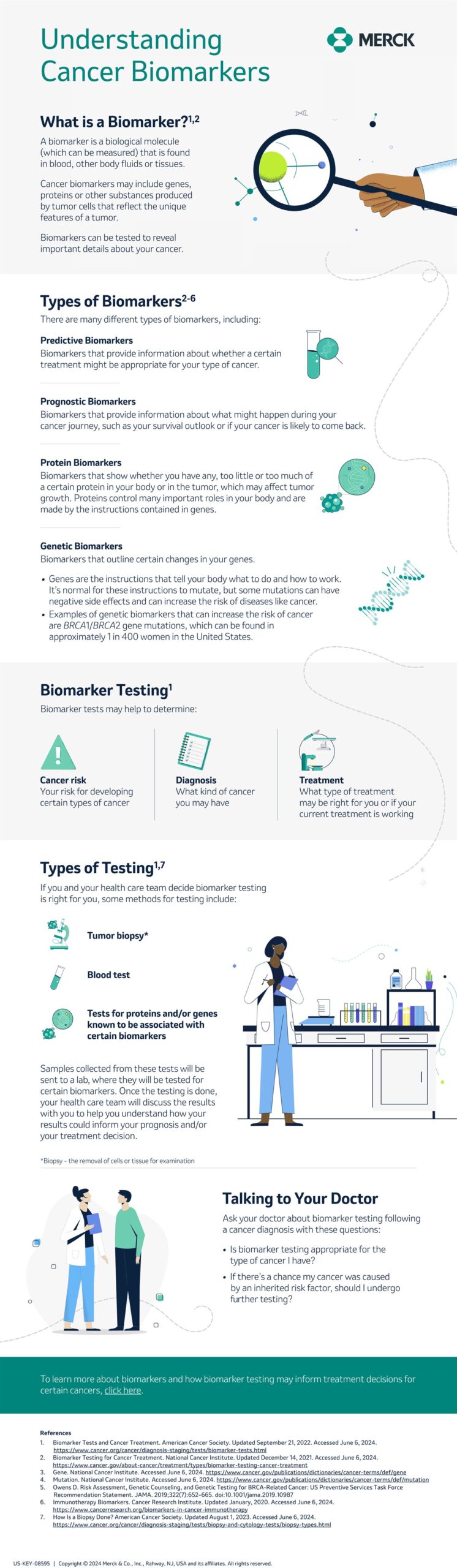
As CDD is caused by a mutation in the CDKL5 gene, genetic testing is required for a diagnosis. With 70-80% of unexplained epilepsy cases now estimated to have a genetic cause, the use of improved genetic testing technologies has assisted in identifying the genes associated with epilepsy in patients and expanding diagnostic utility.
For patients with unexplained epilepsy, genetic testing results may influence their treatment plan, diet, and options to participate in suitable clinical trials for gene-specific studies that further enhance research in the space.
Furthermore, genetic testing is not restricted to pediatric patients. The National Society of Genetic Counselors (NSGC) recommends that all patients with unexplained epilepsy be offered genetic testing regardless of age and periodic reanalysis of prior test results, if needed.
“Finding the best care and resources for the CDD community is crucial to supporting the mental and physical wellbeing of patients and their families,” said John Flatt, M.D., Pediatric Neurologist and Medical Director at Marinus Pharmaceuticals. “I encourage those affected by refractory seizures to discuss the resources available to them with their healthcare team, including genetic testing, treatment options, and counseling, to better understand their or their loved one’s condition and explore tailored approaches to managing their symptoms.”
Confirming a diagnosis of a rare genetic epilepsy disorder such as CDD through genetic testing can help clinicians and families personalize treatment plans and best prepare for the challenges and treatment pathways ahead.
To learn more about CDD, access educational resources from trusted advocacy organizations, and read patient stories, visit the Marinus website, here: https://marinuspharma.com/focus-areas/cdkl5-deficiency-disorder-cdd/.