2024-12-17T09:01:00
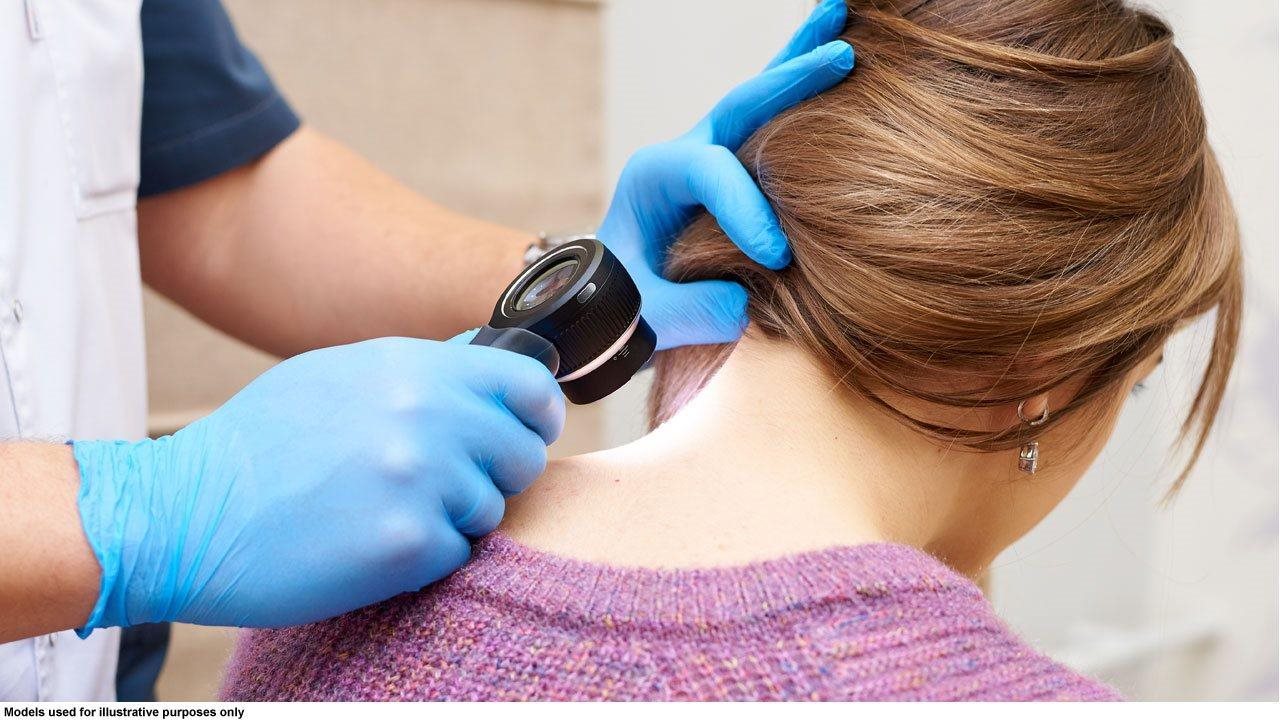
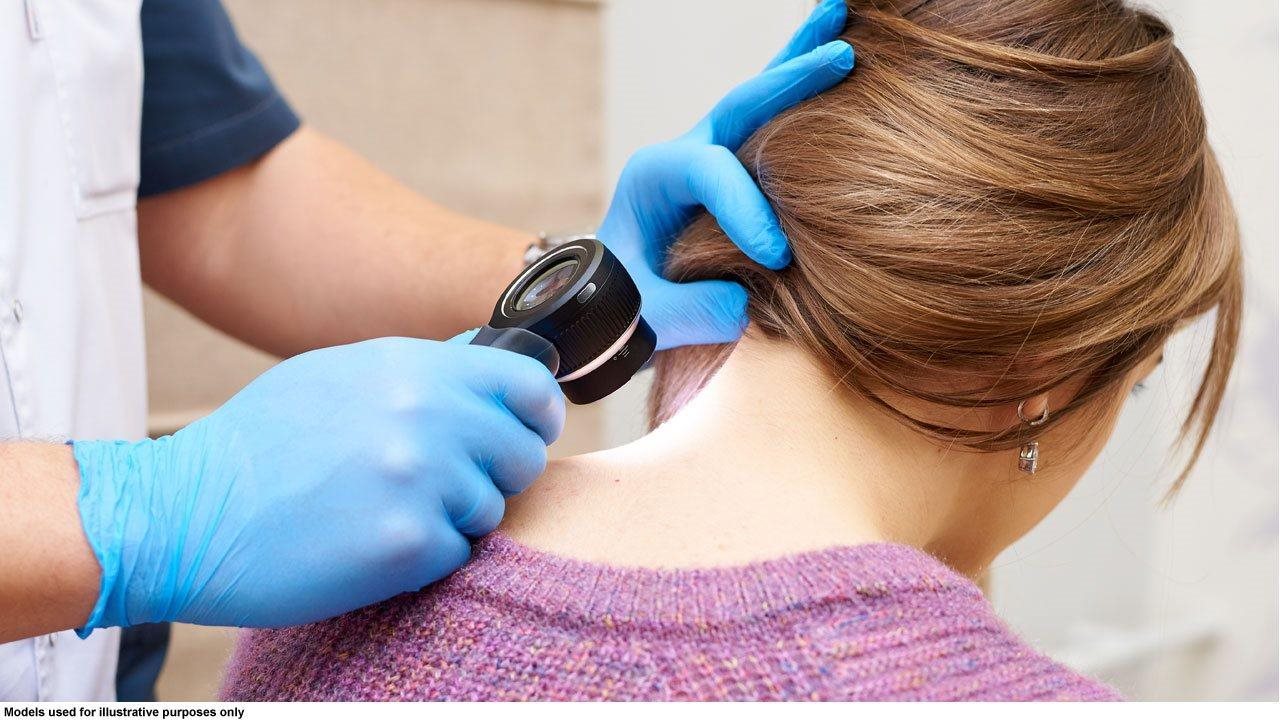
(BPT) – In 2024, more than 100,000 people will be diagnosed with melanoma, a form of skin cancer characterized by the uncontrolled growth of pigment-producing cells called melanocytes located in the skin. When melanoma spreads beyond the surface of the skin to other organs (also known as advancing), it can become deadly, which is why it is important to understand the available treatment options if you or a loved one are facing a melanoma diagnosis.
Melanoma is considered the most serious form of skin cancer because it is more likely to spread to other areas of the body. When someone is diagnosed with melanoma, doctors must determine the stage of the cancer, meaning how much the cancer has spread in the body. As melanoma becomes more advanced, meaning it has spread to other organs, it becomes more challenging to treat and survival rates decline. Of patients newly diagnosed with stage I and II melanomas, stage II makes up approximately 16.5%, and approximately half of these are IIB and IIC.
Fortunately, many melanoma patients have treatment options. Surgery, also known as resection, is what most physicians recommend to treat stage IIB or IIC melanoma. However, about one-third of patients with surgically resected stage IIB and nearly one-half of patients with surgically resected stage IIC melanoma experience recurrence (the cancer coming back) within five years after diagnosis. Due to innovations in the melanoma treatment landscape, immunotherapy can be used to treat eligible melanoma patients after surgery. Immunotherapies are designed to use a patient’s own immune system to help prevent the cancer from coming back.
Adjuvant therapy is an additional cancer treatment given after the primary treatment (or surgery for early-stage diagnosis) to help prevent the cancer from coming back. Thanks to treatment innovations, there are adjuvant immunotherapy options for eligible patients that are designed to use a person’s own immune system to help fight their cancer.
In 2023, Opdivo® (nivolumab) was approved by the U.S. Food and Drug Administration as a prescription medicine used to treat a kind of skin cancer called melanoma. It may be used alone in adults and children 12 years and older with stage IIB, stage IIC, stage III or stage IV melanoma to help prevent melanoma from coming back after it has been completely removed by surgery. This approval provides a treatment option for these melanoma patients that may help prevent their cancer from returning.
Opdivo can cause your immune system to attack normal organs and tissues in any area of your body and can affect the way they work. These problems can sometimes become severe or life-threatening and can lead to death. These problems may happen anytime during treatment or even after your treatment has ended. You may have more than one of these problems at the same time. Serious side effects may include lung problems, intestinal problems, liver problems, hormone gland problems, kidney problems, and skin problems. Call or see your healthcare provider right away if you develop any new or worse signs or symptoms. Please see additional Important Safety Information below.
“Opdivo is a PD-1 inhibitor (a type of immunotherapy) that is indicated as an adjuvant treatment for eligible patients with stages IIB, IIC, III, as well as stage IV completely resected melanoma,” said Hussein A. Tawbi, MD, PhD, Melanoma Medical Oncologist, Department of Melanoma Medical Oncology, Division of Cancer Medicine, The University of Texas MD Anderson Cancer Center.* “This therapy may help prevent cancer from coming back, providing a treatment option and hope for these patients.”
With the cases of melanoma rising worldwide, it’s important to know and understand the different treatment options available to treat early-stage melanoma that can be removed by surgery. “If you or a loved one has been diagnosed with melanoma, you should speak with your healthcare team about your treatment options based on your specific diagnosis,” said Dr. Tawbi. “Adjuvant treatment options, such as immunotherapy, may be an option.”
If you or a loved one is diagnosed with early-stage melanoma, be sure to ask the healthcare team if Opdivo could be a treatment option after surgery. To learn more about Opdivo, visit Opdivo.com.
*Dr. Tawbi has previously served as a clinical trial investigator and scientific advisor to Bristol Myers Squibb.
INDICATION:
OPDIVO® (nivolumab) is a prescription medicine used to treat a kind of skin cancer called melanoma. It may be used alone in adults and children 12 years and older with Stage IIB, Stage IIC, Stage III or Stage IV melanoma to help prevent melanoma from coming back after it has been completely removed by surgery.
It is not known if OPDIVO is safe and effective in children younger than 12 years of age with melanoma or MSI-H or dMMR metastatic colorectal cancer.
It is not known if OPDIVO is safe and effective in children for the treatment of any other cancers.
Important Safety Information for OPDIVO® (nivolumab)
What is the most important information I should know about OPDIVO?
OPDIVO is a medicine that may treat certain cancers by working with your immune system. OPDIVO can cause your immune system to attack normal organs and tissues in any area of your body and can affect the way they work. These problems can sometimes become severe or life-threatening and can lead to death. These problems may happen anytime during treatment or even after your treatment has ended. You may have more than one of these problems at the same time.
Call or see your healthcare provider right away if you develop any new or worse signs or symptoms, including:
- Lung problems: cough; shortness of breath; chest pain
- Intestinal problems: diarrhea (loose stools) or more frequent bowel movements than usual; stools that are black, tarry, sticky, or have blood or mucus; severe stomach-area (abdominal) pain or tenderness
- Liver problems: yellowing of your skin or the whites of your eyes; severe nausea or vomiting; pain on the right side of your stomach area (abdomen); dark urine (tea colored); bleeding or bruising more easily than normal
- Hormone gland problems: headaches that will not go away or unusual headaches; eye sensitivity to light; eye problems; rapid heart beat; increased sweating; extreme tiredness; weight gain or weight loss; feeling more hungry or thirsty than usual; urinating more often than usual; hair loss; feeling cold; constipation; your voice gets deeper; dizziness or fainting; changes in mood or behavior, such as decreased sex drive, irritability, or forgetfulness
- Kidney problems: decrease in your amount of urine; blood in your urine; swelling in your ankles; loss of appetite
- Skin problems: rash; itching; skin blistering or peeling; swollen lymph nodes; painful sores or ulcers in the mouth or nose, throat, or genital area; fever or flu-like symptoms
Problems can also happen in other organs and tissues. These are not all of the signs and symptoms of immune system problems that can happen with OPDIVO. Call or see your healthcare provider right away for any new or worsening signs or symptoms, which may include:
- Chest pain; irregular heart beat; shortness of breath; swelling of ankles
- Confusion; sleepiness; memory problems; changes in mood or behavior; stiff neck; balance problems; tingling or numbness of the arms or legs
- Double vision; blurry vision; sensitivity to light; eye pain; changes in eye sight
- Persistent or severe muscle pain or weakness; muscle cramps
- Low red blood cells; bruising
Getting medical help right away may help keep these problems from becoming more serious. Your healthcare team will check you for these problems during treatment and may treat you with corticosteroid or hormone replacement medicines. Your healthcare team may also need to delay or completely stop your treatment if you have severe side effects.
Possible side effects of OPDIVO
OPDIVO can cause serious side effects, including:
- See “What is the most important information I should know about OPDIVO?”
- Severe infusion reactions. Tell your healthcare team right away if you get these symptoms during an infusion of OPDIVO: chills or shaking; itching or rash; flushing; shortness of breath or wheezing; dizziness; feel like passing out; fever; back or neck pain
- Complications of bone marrow (stem cell) transplant that uses donor stem cells (allogeneic). These complications can be severe and can lead to death. These complications may happen if you underwent transplantation either before or after being treated with OPDIVO. Your healthcare provider will monitor you for these complications.
The most common side effects of OPDIVO, when used alone, include: feeling tired; rash; pain in muscles, bones, and joints; itching; diarrhea; nausea; weakness; cough; vomiting; shortness of breath; constipation; decreased appetite; back pain; upper respiratory tract infection; fever; headache; stomach-area (abdominal) pain; vomiting; and urinary tract infection.
These are not all the possible side effects. For more information, ask your healthcare provider or pharmacist. You are encouraged to report side effects of prescription drugs to the FDA. Call 1-800-FDA-1088.
Before receiving OPDIVO, tell your healthcare provider about all of your medical conditions, including if you:
- have immune system problems such as Crohn’s disease, ulcerative colitis, or lupus
- have received an organ transplant, including corneal transplant
- have received or plan to receive a stem cell transplant that uses donor stem cells (allogeneic)
- have received radiation treatment to your chest area in the past and have received other medicines that are like OPDIVO
- have a condition that affects your nervous system, such as myasthenia gravis or Guillain-Barré syndrome
- are pregnant or plan to become pregnant. OPDIVO can harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if OPDIVO passes into your breast milk. Do not breastfeed during treatment with OPDIVO and for 5 months after the last dose of OPDIVO.
Females who are able to become pregnant:
Your healthcare provider should do a pregnancy test before you start receiving OPDIVO.
- You should use an effective method of birth control during your treatment and for 5 months after the last dose of OPDIVO. Talk to your healthcare provider about birth control methods that you can use during this time.
- Tell your healthcare provider right away if you become pregnant or think you may be pregnant during treatment with OPDIVO.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Please see U.S. Full Prescribing Information and Medication Guide for OPDIVO.
©2024 Bristol-Myers Squibb Company. OPDIVO® is a registered trademark of Bristol-Myers Squibb Company.
1506-US-2400473 12/24